scott@vtx-cpd.com
Forum Replies Created
-
AuthorPosts
-
Replying to Catriona Edgar 09/01/2023 - 21:11
Hello Catriona!
I am typing this message from Ayrshire too! We love just outside Galston!
Thank you for joining. I really hope you enjoy the course.
Scott 🙂
Replying to Alison Lambert 08/01/2023 - 20:53
Hello Alison!
Really lovely to see you here! Thank you so much for supporting the course.
I really hope you ennjoy the content. Let me know if you have any questions.
Scott 🙂
Replying to adele smart 04/01/2023 - 18:06
Hey pal.
Hope you are well and Happy New Year!
It is a grim read! It was the sheer number of cases that surprised me too!
Scott x
Hello Raquel.
I hope you are safe and well. Happy New Year!
I have popped some thoughts under your questions below:
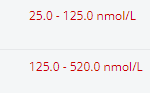
Wanted to double check. The Idexx lab range for cobalamin states that normal is from 284-836ng/L. Is it still recommended to supplement in animals with clinical signs when it has been below 400ng/L as you had advised in your course.
“Short answer… YES! Cobalamin should be supplemented whenever serum cobalamin concentration is subnormal. There is a 12% probability that dogs with low-normal serum cobalamin concentration (ie, less than approximately 400 ng/L) might also benefit from supplementation. Supplementation of Vitamin B12 is recommended when the cobalamin is low or low normal (< 400 ng/L), in addition to treatment of the underlying cause." Second question-1) why is it that Idexx uses a different reference range as normal? "Good question... short answer is... we are still learning. Reference ranges are established as they are, I am sure they will change with time." 2) for animals who have their cobalamin levels rechecked after the parenteral supplementation protocol. If the cobalamin is still below 400 ng/L but within the “284-836 mg/L” normal range. Then do I take it as the cobalamin levels as subnormal or normal at that point? Just in terms of knowing how I should supplement it going forward. "If the levels are still below 400 after supplementation, I would take that as abnormal and continue supplementation" I hope that helps. Scott 🙂
Replying to Claire H. 05/01/2023 - 01:56
Hello!
Brilliant suggestion… on it!
Scott 🙂
Replying to Kathryn B. 11/12/2022 - 21:09
Hello!
Happy New Year. Thank you as always for all of your brilliant questions and on-going support. I have popped some thoughts under your questions below:
– at the start of a d+ work up would it be worth just testing for parasites and Giardia, rather than bacteria given how difficult interpretation of bacteria can be? Then revisit bacterial testing later on if still no diagnosis. Or would you still test for everything at the get go?
Hmmmm. This is a really good question. I feel the biggest issue is that we will often detect organisms that are not actually significant. Campylobacter is a good example of this. I always question the significance and always presume there is a chronic enteropathy underlying it all! I think there is probably more justification for faecal analysis in younger dogs. I would always consider parasitology in every case. I must admit that in my chronic GI cases, I will give them 7 days of fenbendazole regardless! This paper is helpful!
https://pubmed.ncbi.nlm.nih.gov/33277779/
– if you treat a positive faecal culture, be that parasitic/Giardia/bacteria, would you re-test a faecal sample at the end of the treatment course or just go by clinical cure?
Honestly. I would 100% go with how the clinical signs are. If the clinical signs resolve, I would not re-culture. I think it can end up confusing us more!!! I would be most careful when using the faecal antigen to monitor. The antigen will remain positive despite resolution of Giardia. If you are following up Giardia, I would use parasitology/floatation for monitoring.
– would you interpret faecal culture differently in a raw fed dog vs. commercially fed dog?
I think that the data show us that raw fed dogs probably will culture more pathogens:
https://pubmed.ncbi.nlm.nih.gov/35191029/
https://pubmed.ncbi.nlm.nih.gov/35923819/I am not sure how much it would affect my interpretation. Even if there was Salmonella or Campylobacter there… the interpretation would always depend on clinical signs. \i would only ever treat the Salmonella if there was significant haemorrhagic diarrhoea and systemic disease.
– do you have any good stats I can fire at owners about what % GI cases will improve on diet trial alone. It’s like they don’t want their pet to have a problem that will respond just to diet change – they want something more exciting! I find it so difficult to get people on board, they just seem to decide it’s a waste of time without even starting it
Typically, response to diet was higher than 60% and reached 100% except for one study reporting a remission of clinical signs in 45% of dogs:
https://onlinelibrary.wiley.com/doi/10.1111/j.1939-1676.2010.0632.x
https://pubmed.ncbi.nlm.nih.gov/19750741/– if you give a probiotic at the same time as an antibiotic, would that supercharge any resistant bacteria?!
Hmmmmmm… Good question! I don’t think so! It is more likely that the probiotics will protect against the dysbiosis caused by the antibiotics. I think using them together is a positive thing!
– what doses would you give for Sivomixx and VSL3 please, I’ve not used these before?
I will post the dosing chart separately!
– is there any evidence for feeding dogs with GI dz the faeces of a heathy dog?
Generally speaking FMT is given as an enema per rectum, However there are some case reports of oral administration:
https://pubmed.ncbi.nlm.nih.gov/35859811/
So, I think the evidence for this is limited, but definitely a possibility.
– I’ve worked with a lot of vets who give a one of jab of Betamox and dex to acute GI patients. Is there any evidence for/against the one off dex? (obviously wouldn’t give the Betamox!)
Me too! I also did this for years! There is no evidence for this. My suspicion would be that most cases would have self-resolved despite the dexamethasone. However, there is probably inflammation involved in these cases… so it may have helped!
Hope that helps.
Scott 🙂
Replying to Kathryn B. 11/12/2022 - 21:09
Hello!
Happy New Year. Thank you as always for all of your brilliant questions and on-going support. I have popped some thoughts under your questions below:
– at the start of a d+ work up would it be worth just testing for parasites and Giardia, rather than bacteria given how difficult interpretation of bacteria can be? Then revisit bacterial testing later on if still no diagnosis. Or would you still test for everything at the get go?
Hmmmm. This is a really good question. I feel the biggest issue is that we will often detect organisms that are not actually significant. Campylobacter is a good example of this. I always question the significance and always presume there is a chronic enteropathy underlying it all! I think there is probably more justification for faecal analysis in younger dogs. I would always consider parasitology in every case. I must admit that in my chronic GI cases, I will give them 7 days of fenbendazole regardless! This paper is helpful!
https://pubmed.ncbi.nlm.nih.gov/33277779/
– if you treat a positive faecal culture, be that parasitic/Giardia/bacteria, would you re-test a faecal sample at the end of the treatment course or just go by clinical cure?
Honestly. I would 100% go with how the clinical signs are. If the clinical signs resolve, I would not re-culture. I think it can end up confusing us more!!! I would be most careful when using the faecal antigen to monitor. The antigen will remain positive despite resolution of Giardia. If you are following up Giardia, I would use parasitology/floatation for monitoring.
– would you interpret faecal culture differently in a raw fed dog vs. commercially fed dog?
I think that the data show us that raw fed dogs probably will culture more pathogens:
https://pubmed.ncbi.nlm.nih.gov/35191029/
https://pubmed.ncbi.nlm.nih.gov/35923819/I am not sure how much it would affect my interpretation. Even if there was Salmonella or Campylobacter there… the interpretation would always depend on clinical signs. \i would only ever treat the Salmonella if there was significant haemorrhagic diarrhoea and systemic disease.
– do you have any good stats I can fire at owners about what % GI cases will improve on diet trial alone. It’s like they don’t want their pet to have a problem that will respond just to diet change – they want something more exciting! I find it so difficult to get people on board, they just seem to decide it’s a waste of time without even starting it
Typically, response to diet was higher than 60% and reached 100% except for one study reporting a remission of clinical signs in 45% of dogs:
https://onlinelibrary.wiley.com/doi/10.1111/j.1939-1676.2010.0632.x
https://pubmed.ncbi.nlm.nih.gov/19750741/– if you give a probiotic at the same time as an antibiotic, would that supercharge any resistant bacteria?!
Hmmmmmm… Good question! I don’t think so! It is more likely that the probiotics will protect against the dysbiosis caused by the antibiotics. I think using them together is a positive thing!
– what doses would you give for Sivomixx and VSL3 please, I’ve not used these before?
I will post the dosing chart separately!
– is there any evidence for feeding dogs with GI dz the faeces of a heathy dog?
Generally speaking FMT is given as an enema per rectum, However there are some case reports of oral administration:
https://pubmed.ncbi.nlm.nih.gov/35859811/
So, I think the evidence for this is limited, but definitely a possibility.
– I’ve worked with a lot of vets who give a one of jab of Betamox and dex to acute GI patients. Is there any evidence for/against the one off dex? (obviously wouldn’t give the Betamox!)
Me too! I also did this for years! There is no evidence for this. My suspicion would be that most cases would have self-resolved despite the dexamethasone. However, there is probably inflammation involved in these cases… so it may have helped!
Hope that helps.
Scott 🙂
Replying to Kerida Shook 28/11/2022 - 11:58
Hello.
I think the jury is still out regarding the anagesic effect of maropitant. More work to be done regarding the single dose that you mention. Having said that, there are some papaers suggesting a benefit:
https://pubmed.ncbi.nlm.nih.gov/33950785/
Hope you have had a lovely Christmas.
Scott 🙂
So excited about this!
Welcome to the team Felipe!
Scott 🙂
Very excited about this!
Welcome to the team Felipe!
Scott 🙂
Replying to Marit Veeber 25/12/2022 - 11:41
Hello Marit!
Lovely to hear from you! I am glad you have found some time to finish the course.
The numbers vary a little depending on what study you look at. I was referencing an average. This study is quite helpful:
https://pubmed.ncbi.nlm.nih.gov/30246401/
Hope that helps.
Scott 🙂
Replying to Raquel M. 21/12/2022 - 19:44
Hello Raquel!
I hope you mangaed to join and enjoyed the session.
Question is… will you use prazosin?
Scott 🙂
Replying to Liz Bode 08/12/2022 - 19:56
That is really helpful Liz.
I have a similar approach, I just wanted to make sure I was not missing a trick!
Scott 🙂
Replying to Clare McConville 03/11/2022 - 17:41
Hello.
Hope you are well. The dog is still alive and had an ACTH stimulation test… very Addisonian!
I was just so shocked that the potassium was a real result! Good outcome for dog though!
Scott 🙂
-
AuthorPosts