scott@vtx-cpd.com
Forum Replies Created
-
AuthorPosts
-
Replying to Laura S. 23/03/2025 - 13:28
Hi Laura,
I know, right? There really are so many positive anecdotal reports. It does make you wonder whether we’re seeing a bit of a placebo effect, or if some of the benefit is just from the saline or the act of flushing itself. Either way, it looks like we’re back to trusty saline for now.
Re the nebuliser, yes, absolutely. LOVE a nebuliser. My favourite for cats is the BreathEzy one as it’s really quiet, which makes a huge difference for feline compliance. I’ve had a few chronic rhinitis cases where the owners bought their own, but I’ve also worked in clinics that loaned them out with a deposit system, which can be a really good solution for short-term use.
The one I showed in the lecture was the Philips InnoSpire Essence, which is a reliable tabletop compressor. It was paired with either a Flexineb or Aeromask in the photo. These masks are designed for equine use originally, but they adapt well to cats and small dogs. You can usually source them via vet supply companies or equine suppliers.
Here’s the Flexineb link I mentioned: https://www.breatheazy.co.uk/product/cats/flexineb-c2/
Let me know if you want any more info or links.
Scott 🙂
Replying to Laura S. 23/03/2025 - 13:28
Hi Laura,
I know, right? There really are so many positive anecdotal reports. It does make you wonder whether we’re seeing a bit of a placebo effect, or if some of the benefit is just from the saline or the act of flushing itself. Either way, it looks like we’re back to trusty saline for now.
Re the nebuliser, yes, absolutely. LOVE a nebuliser. My favourite for cats is the BreathEzy one as it’s really quiet, which makes a huge difference for feline compliance. I’ve had a few chronic rhinitis cases where the owners bought their own, but I’ve also worked in clinics that loaned them out with a deposit system, which can be a really good solution for short-term use.
The one I showed in the lecture was the Philips InnoSpire Essence, which is a reliable tabletop compressor. It was paired with either a Flexineb or Aeromask in the photo. These masks are designed for equine use originally, but they adapt well to cats and small dogs. You can usually source them via vet supply companies or equine suppliers.
Here’s the Flexineb link I mentioned: https://www.breatheazy.co.uk/product/cats/flexineb-c2/
Let me know if you want any more info or links.
Scott 🙂
Hi Raquel,
Yes, I’ve looked into the KeyScreen™ GI Parasite PCR from Antech. It’s a multiplex PCR that screens for 20 intestinal parasites from a single fecal sample and reportedly detects 2x more infections than standard in-clinic fecal flotations (O&P), which could be really helpful in those low-burden or intermittent shedding cases.
Some useful features:
Detects benzimidazole resistance in hookworms, which can guide treatment choices
Flags the zoonotic potential of Giardia
Offers fast, sensitive detection for earlier intervention
It also aligns with CAPC recommendations for routine parasite testing—four times in the first year for puppies/kittens and one to two times per year for adults, depending on lifestyle and risk factors.That said, I’m struggling to find a clear list of exactly which parasites it includes. Do you know? I get the impression it’s more focused on parasites and worms, whereas the IDEXX faecal PCR panels seem more geared toward bacterial pathogens (like Campy, Salmonella, Clostridium, etc.). If that’s the case, this might actually be a useful complementary test, especially in routine or preventive care. I haven’t personally used it yet, though.
Best,
Scott
Replying to Raquel M. 19/03/2025 - 15:18
Hi Raquel,
Thanks so much for your reply — it was really interesting to hear your perspective, especially with your experience working in the Caribbean and having trained in the UK. I can imagine the shift in disease prevalence must have been quite an adjustment!
Your approach sounds really sensible and practical. I think it’s reassuring that a positive heartworm result in an asymptomatic dog doesn’t necessarily mean surgery has to be cancelled, especially when there are no signs of advanced disease or cardiac changes, and you’ve got informed consent. I’ve also come across the recommendation to avoid elective surgery during heartworm treatment, but like you, I’m not sure how much actual data backs it up — it’s mentioned on VIN and elsewhere, but I’d love to see more specific studies to guide us.
The ehrlichiosis side of things is equally interesting. I haven’t come across any formal studies specifically looking at the benefits of screening before elective procedures, but your anecdotal experience highlights a real-world need for it in endemic areas. I presume the bleeding you saw was due to thrombocytopenia? That seems to be the key issue with E. canis in a surgical context.
The challenge with screening, of course, is that many patients may have positive serology but not be clinically affected — so I wonder if it might be more useful to simply perform a blood smear and haematology ahead of surgery and screen specifically for thrombocytopenia. That feels like a more targeted and clinically relevant approach, especially in settings where broad screening for tick-borne disease isn’t practical. It could help identify dogs at risk of bleeding without overinterpreting past exposure.
If I come across any studies on this topic, I’ll definitely share them here. Thanks again for such a thoughtful and insightful reply — it’s great to learn from your experience.
Scott 🙂
Sorry!
One more random question… how exactly is it that they do the palatability work? Do they do it with sick or well animals?
I know they pay humans to taste food… but never thought about how this works for our patients. Most of the prescription diets are for ‘sick’ animals so must be tricky to do palatability in these populations?
Scott 🙂
Replying to Georgia 21/03/2025 - 15:55
Very helpful!
Thank you!
Scott 🙂
Replying to Georgia 21/03/2025 - 16:00
Thanks for the reply!
I did see that JFMS had just published this article this week:
https://pmc.ncbi.nlm.nih.gov/articles/PMC11874005/pdf/10.1177_1098612X251320877.pdf
Scott 🙂
Replying to Laura S. 21/03/2025 - 18:03
Hi Laura,
Ah, thank you for sharing this. I’m genuinely disappointed (and a little deflated) to read the JFMS study. It very much doesn’t support the use of intranasal maropitant, despite all the anecdotal promise and theoretical basis we’d been leaning on. I had completely missed this paper, so I really appreciate you and your colleague bringing it to the table.
So now we’re left in a tricky spot. The evidence says “no benefit,” but part of me still wonders if there’s a place for it in the most refractory cases, where we’re trying to do something to help these poor cats breathe. Of course, any use now really has to be framed as off-label and not evidence-supported, and I think this study will rightly temper some of the optimism that’s been floating around.
Thanks again for sharing. I’ll share it in other forums too.
Scott 🙂
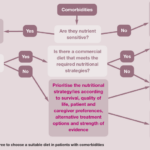
This is a great question!
I must admit I often panic. I find myself prioritising the most life threatening issue… but I fear that this may be the wrong approach!
I think the one that probably comes up most for me is kidney. For example, I have a patient at the moment with chronic kidney disease but also some really severe skin issues/allergies. The other one that comes up quite a bit is when patients are on a hydrolysed protein for GI issues and then develop another problem.
I often will call the food companies. I find Hills and RC very helpful! I feel less people go for the home cooked/formulated option but I always offer it.
Scott 🙂
Replying to Georgia 17/03/2025 - 09:45
Love the fibre chat!
I do tend to recommend a lot of people to add psyllium or pumpkin to the diet. What are your thoughts on pumpkin? Also, with the psyllium, what amounts do you normally recommend?
There are a few veterinary fibre blend supplements out there too, I think Protexin might make one. What do you think of those?
Scott 🙂
Replying to Raquel M. 20/03/2025 - 12:34
I think that is a great questions generally!
I always try and advocate charging for this sort of time. We have a cost for a technician appointment. It is around $50 Canadian Dollars. This would normally be what we charge for this sort of thing.
If this is for a patient that has been hospitalised or been in for a procedure we would often do it as part of the discharge process without additional charge.
Scott 🙂
Hi Kerida,
Hope you’re doing well! How’s life in practice treating you?
With rectal diazepam becoming unavailable, a lot of us are turning to intranasal midazolam as an alternative for at-home seizure management in epileptic dogs. There’s good evidence supporting its use, with studies showing it achieves faster seizure cessation than rectal diazepam and tends to have fewer adverse effects. A study in the Journal of Veterinary Internal Medicine found that intranasal midazolam was as effective as rectal diazepam in managing canine status epilepticus, which you can read more about here: https://pubmed.ncbi.nlm.nih.gov/28543780/.
For administration, the standard dose is 0.2 mg/kg intranasally using a mucosal atomization device, which ensures good absorption. This is backed by research discussing the various administration routes of benzodiazepines in dogs: https://pubmed.ncbi.nlm.nih.gov/33663513/.
Rectal diazepam tablets are not recommended for rectal administration due to inconsistent absorption and efficacy. A systematic review with meta-analysis highlights the effectiveness of non-intravenous midazolam compared to rectal diazepam: https://pubmed.ncbi.nlm.nih.gov/25817929/.
The big advantages of intranasal midazolam are its rapid onset and ease of use. Since it’s absorbed quickly via the nasal mucosa, it tends to work faster than rectal diazepam, which is crucial in an emergency. The Journal of Veterinary Internal Medicine study backs this up: https://pubmed.ncbi.nlm.nih.gov/28543780/. It’s also a lot easier for owners to administer, especially compared to trying to give something rectally mid-seizure. This is further discussed in the review on benzodiazepine administration: https://pubmed.ncbi.nlm.nih.gov/33663513/.
If you’re switching owners to intranasal midazolam, it’s worth taking some time to train them on how to use the atomization device properly. They also need to know what to look out for in terms of side effects, like sedation or nasal irritation, and when to seek further veterinary care if seizures persist.
Overall, intranasal midazolam seems to be a reliable and effective alternative to rectal diazepam for at-home seizure management. It’s great to have a practical option that works well in these cases.
Hope that helps. Let me know how you’re getting on.
Scott 🙂
Replying to Gemma B. 19/03/2025 - 15:38
Hey Gemma!
This is really interesting. I wonder what is is about the j/D that makes it more palatable?
I suppose my question would be… why do they not just add that to all the kidney diets!?
Scott 🙂
Replying to Raquel M. 19/03/2025 - 15:50
Hey Raquel.
You can access the recording here:
https://vtx-cpd.com/webinars/?filter=Caesarean
Scott 🙂
Replying to Raquel M. 19/03/2025 - 21:17
Thanks Raquel.
I think the time element is one of the biggest issues.
This is definitely not the sort of thing that can we rushed.
We will often book a separate appointment just to go through training and using the inhaler.
Scott 🙂
-
AuthorPosts