Liz Bode
Forum Replies Created
-
AuthorPosts
-
Replying to scott@vtx-cpd.com 17/09/2023 - 19:15
Hi Scott
It’s available in the human medicine world but as far as I’m aware we don’t use it in veterinary yet. As I said, it’s a pilot study so much more data is needed before it becomes mainstream 😉
Liz
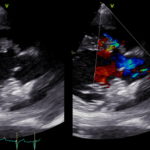
I agree! The systolic function looks OK and so excludes DCM. A congenital condition is very likely here. SAS usually causes concentric hypertrophy, which isn’t present, but at end-stage SAS you get what we call ‘myocardial mismatch’ or ‘afterload mismatch’ where the walls actually become thinner due to replacement fibrosis. So, you could see normal/ thin walls with even severe SAS. In my mind though this left side looks volume loaded, so we are thinking about a disease process that is congenital and causes volume loading of the left side…it will become clear (hopefully) with these videos…what do you think now?
https://drive.google.com/file/d/1UJWZeF3nPodqAGy01Bh4YdXkG2NyaZi7/view?usp=drive_link
https://drive.google.com/file/d/1G1Kvx4VC2ehmTTHMkcXNVe_vd1sYk5K9/view?usp=drive_linkIn terms of the interatrial septum, you often get echo dropout around the middle of the septum. If you think there is an ASD you need to identify it on 2 views to make sure it isn’t an artefact 🙂
Hi Natalie,
Some great questions, treating cats is confusing with little or no evidence for very much!! I will answer each question in turn:
My understanding from the lectures is that all cats in congestive heart failure get frusemide at lowest effective dose.
Yes, that’s correct. We will cover this later in the CHF section. However, as a rule of thumb I use 2mg/kg PO BID (TID if they were difficult to control) and then once I am happy the cat is stable I will try and reduce the dose to lowest effective, although not really below 1mg/kg BID.Those with evidence of smoke / spontaneous contrast on echo get clopidogrel to reduce risk of thrombus.
Yes, clopidogrel is the one we choose as we have evidence for its use from the FATCAT study (2015) in recurrent ATE events. So, I prescribe it to cats with moderate dilation of the LA, smoke, or poor LA systolic function.Do you ever use aspirin in these cases?
Not really, no. the therapeutic index isn’t very high (its not COX selective) and I would prefer to use clopidogrel with rivaroxaban (a factor Xa inhibitor) or one or the other. I might use aspirin if the cat is very difficult to tablet though, as better than nothing probably (although we don’t know this either!).I know a lot of clinicians use every third day (think it’s a quarter tablet?). Can this be given in combination with clopidogrel?
Yes, you can use it in combination with clopidogrel as they work in different ways.You said there’s no good evidence that ACE inhibitors such as benazepril improve survival so we should not give these unless hypertensive?
I will use an ACE inhibitor if the cat isn’t doing very well, but the King paper suggests that including an ACE inhibitor has no benefit either before CHF develops or during CHF. I will use spironolactone though as there is a (poor) study that suggests some benefit, but what I really use it for is boosting the potassium levels.And pimobendan is contraindicated unless it is DCM which is much rarer.
It’s not contraindicated per se, it is just that there is no evidence that it works. This makes sense as pimobendan increases contractility but HCM is a diastolic disease. a recent paper showed no benefit in using it in cats with HCM to 180 days, so it is going out of fashion. I would definitely use it in a cat with DCM though, or possibly end-stage HCM where you see poor systolic function secondary to myocardial ischaemia.Then where I’m a little confused is – do you use beta blockers such as atenolol only in obstructive hypertrophic cases where there is systolic anterior motion, and then diltiazem in HCM cases without obstruction to improve diastolic filling? Or am I mixed up?
Yes, atenolol only in severe HOCM. Again, no benefit here but physiologically it makes sense to use a beta blocker. You need to demonstrate the severity of the obstruction via Doppler though before prescribing it. We don’t use diltiazem in cats, unless they have an arrhythmia. It used to be prescribed for HCM as the thought was that slowing the HR down would improve myocardial perfusion, but it is TID dosing and there is no evidence that it works.Hope that clears things up for you 🙂
Liz
Hi Natalie,
So there is one loop only (I’m on holiday this week but will add more next week once I’ve got my laptop). In this loop you can see left atrial and ventricular dilation with normal systolic function. There is also AF on the ECG. The MV is slightly thickened but isn’t the concern in this dog. Any other thoughts as to processes that could cause these findings in a dog with a loud murmur?
Liz
Replying to Natalie Niven 07/09/2023 - 17:01
Hi Natalie,
I’ve not seen one performed in dogs, only people, but the procedure is the same for both. They use cardioplegia and then place catheters within various vessels and circulate the blood through the bypass machine. The heart is approached via the left atrium and as this is a low pressure chamber with thin walls you can suture it up with little risk, but yes that will always be a risk. The main risk though is thrombosis following recovery and these dogs are given clopidogrel to prevent it. They then repair the valve by placing new chordae to tether the valve again.
Yes, with decompression that is what you do. 30% have R CHF afterwards, but this is easier to manage than L. 30% close up. We don’t have any evidence as to whether they do better than meds alone but this technique is used in people too.
Scott – that’s a great episode of Grey’s!
Liz
Hi everyone
Great to have you all join us on this course. I’m Liz, one of the directors of vtx but also a specialist in cardiologist working in private practice in the NW of England. Please feel free to ask me anything cardio related.
Liz 🙂
Replying to scott@vtx-cpd.com 03/09/2023 - 20:11
Yes, they were the pioneers of the approach and for realising replacement was not as good as repair in dogs in terms of survival post surgery.
Replying to scott@vtx-cpd.com 30/08/2023 - 10:52
Hi Scott,
We haven’t had a suitable candidate yet, but we would certainly be able to try left atrial decompression in a suitable stage C/D candidate.
Repair would be my overall preference, they are having some good outcomes with reverse remodelling and many come off medications. TEER is similar in USA but is in the very early stages in UK.
I haven’t sent any dogs yet, cost is almost prohibitive for many owners in UK where they are not used to paying such high bills for health care vs the USA.
Liz
Replying to scott@vtx-cpd.com 29/08/2023 - 14:20
Hi Scott
That’s hard to answer. If o hear a right sided systolic murmur in a cat I will try and press less hard to see if the murmur goes away. The same when I’m performing echo, if I see turbulence in the RV outflow tract I’ll try and press less hard to see if the turbulence resolves.
Liz
Replying to scott@vtx-cpd.com 29/08/2023 - 16:56
Hi Scott
Unfortunately for the owner it was detected 3 weeks after he rescued him at a routine vaccination. The dog is asymptomatic at present 🙂
Liz
Hi Lauren
Great to have you join us and I’m pleased you’re enjoying it so far.
For a PDA you can see them both on the right parasternal short axis view optimised for the PA and the left cranial view again optimised for the PA. I find the left cranial view gives you much clearer images than the right sided ones though. The trick is to put your probe right where you feel a thrill and then with a few small adjustments it usually comes into view. If you can’t see the whole thing you can often appreciate the flow across it on colour or with continuous wave Doppler.
Liz
Hi Nadine,
Thanks for the question. I tend to avoid it because it increases the risk to the cat (albeit small) and the cost for the owner. I find that 75% of cats will tolerate a complete echo with 2 handlers in a quiet dark room fine. About 15% will need gabapentin prior to the echo, a small number will benefit from butorphanol on top and then the remainder will need the combination you describe. We know that the combination affects very little systolic function etc but it will make HOCM more challenging to identify.
Liz
Replying to Steph Sorrell 21/08/2023 - 09:51
Hi everyone,
Very excited to be on this course with the lovely and knowledgable Steph 🙂
Any cardio questions I’m more than happy to answer.
Liz
Replying to scott@vtx-cpd.com 19/08/2023 - 07:09
Hi Fran
Good question! I’m not 100% sure about the reason but several studies have demonstrated that it is poor at detecting patent infections, unless used in combination with an ELISA. This is presumably due to the amount of DNA present in blood when the adult worms are there vs when the larvae are migrating through the body.
Liz
Replying to Nadine S. 08/08/2023 - 10:41
Hi Nadine,
Welcome to the course.That’s great with regards your echo, congenitals are more complex overall so makes sense to refer these, and I am glad you enjoyed the first lecture.
Liz
-
AuthorPosts