Liz Bode
Forum Replies Created
-
AuthorPosts
-
Hi Julia,
This sounds like a tricky case indeed.
It could be an LA rupture, if the effusion was big enough it might have been causing some limitation to LA size/ the left side might be under-filled due to blood loss. However, normally dogs with LA rupture have significant LA dilation, which is what leads to wall thinning. Often, but not always, you will see a thrombus within the pericardial space as one clue. I think B-lines around the pericardial sac can be misleading. There is a paper that suggests they are conducive to CHF, but in my experience you frequently see B-lines around the heart in normal dogs.
I guess in this case, where I wasn’t sure of the cause but there was significant effusion with tamponade I would attempt to drain it, monitoring carefully for the appearance of a thrombus, so doing it ultrasound guided would be preferable here.
Poor dog, sounds like she was quite poorly!
Liz
Replying to Julia Biernat 20/02/2026 - 12:31
No problem at all!
Yes, it is always a good one to warn owners about. I always say that some ‘idiopathic’ cases will be mesothelioma in the end and we do not have a good way of identifying which cases have it and which don’t!
Replying to Silvana S. 21/02/2026 - 19:46
Hi Silvana,
Welcome, we are really pleased that you have joined us and are starting to use the platform etc. Those are some great suggestions, and we can certainly look to incorporate more of those topics over the next year.
Let us know if you have any further suggestions/ queries or if we can help at all.
Liz
Replying to Ornella R. 15/02/2026 - 21:59
Hi Ornella,
Glad you have found it useful.
Each lecture should have it’s own downloadable pdf? If you can’t access them please let us know.
Liz
Replying to Annet Krabbenborg 16/02/2026 - 12:57
Hi Annet,
Good question! Yes, they have been shown to have larger LV than other dogs. We would still use the EPIC criteria though to determine when to start pimobendan, but we might reassure some owners that the LV isn’t that big in reality!! It is confusing. The study wasn’t one looking at CKCS in particular, but Mark Rishniw demonstrated that as a breed CKCS have LV that are often larger then the 1.7 EPIC cut off!
This was the paper:
https://www.sciencedirect.com/science/article/abs/pii/S1760273422000595?via%3Dihub
Liz 🙂
Replying to Ornella R. 15/02/2026 - 21:51
Hi Ornella,
When measuring turbulent jet velocity: we identify the jet with colour doppler and in order to get an accurate velocity, we place the CW gate in the neck of the jet (vena contracta), is this correct?
Yes, that is correct, or just on the atrial side of the valve within the colour variance if there is TR or MR.
When measuring PA and AO velocities with CW or PW: do we place the cursor gate across the valve, just below or just above?
This depends on where you see the colour variance start. For the most part the turbulent flow will be within the major artery you are looking at, so the gate is placed on the arterial side (rather than the ventricular). However, sometimes, like in R2A, the turbulent flow might start just before the valve in the outflow tract. Then you would place your cursor in that area. It won’t matter with CW as you are measuring the whole way down the cursor, but it will matter with PW (although usually the flow is too fast for PW).
I know that for TV or MV PW we place the gate at the tip of the valve leaflets, does this apply for the PV and AV?
This is only for E and A waves, so this will only apply to inflows, otherwise for regurgitation you place the cursor as above 🙂
Hi Julia,
Mesothelioma is so tricky!! It is REALLY hard to diagnose and can even be missed on histopathology, although there has been some work around immunohistochemistry use, but this is still pretty limited. Therefore, even if you have histopathology of the pericardium/ pleura it won’t always show mesothelioma. It is something I warn owners about. It is also very difficult to treat, you can perform intra-cavitatory chemotherapy (this is what they do in people), but my experience of that is limited I’m afraid (mainly because by the time dogs are diagnosed most owners will choose euthanasia). Survival is varied – some dogs will have aggressive disease and others will have a more protracted course, the use of pleural ports can be useful in some cases. Unfortunately, by the time it is diagnosed it is usually affecting the pleura and pericardium. If it is just pericardial, we can’t remove the whole pericardium due to its association with the base of the heart so it is a nasty neoplasm to have!
Hope that is useful.
LizReplying to Ornella R. 08/02/2026 - 19:05
Hi Ornella,
I would need to look at her file again to be sure, but I don’t think we found a cause and, given the prognosis, the owners didn’t want to investigate very much. We did the standard UPC and this was WNL, no evidence for Cushing’s either.
Sorry I can’t answer that one!
Liz
Replying to Ornella R. 08/02/2026 - 19:18
HI Ornella,
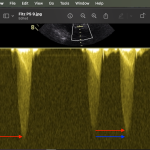
Thanks for the question. Generally you will get a dense appearing profile (termed the ‘chin’) and a fainter area of spectral broadening (termed the ‘beard’). We measure the velocity to the chin and ignore any of the fluffy-stuff that will make the velocity faster than it is. In the attached image the red arrows are the chin and blue the beard.
Hope that is helpful.
Liz
Replying to Annet Krabbenborg 19/01/2026 - 21:34
and here you go for these ones:
Which ultrasound do you prefer for cardiac scans?
Do you mean which machine? I use a GE Vivid and I like the GE machines, but the Philips one give really nice 2D images too. If you mean probe than a phased array probe.
And how much time do you think is reasonable to book off for a heart scan, report and make a plan? Of course should get quicker with practise…
Yes, of course it gets quicker and easier with practice.A straightforward MMVD could take me a total of 20 minutes to echo both sides, measure and report! I guess intially an hour per scan/ measure and report would be about right, depending on how many you do in a day that would leave you time to catch up etc.And when is it useful to do pa vti? Is that when checking pulm flow/check re pulm hypertension?
VTI I mainly use that to look at the severity of PS, looking at the ratio of aortic vs pulmonic VTI. I also use it for shunt ratios. I don’t tend to use it for PHT and I don’t use it every day.🙂
Replying to Annet Krabbenborg 18/01/2026 - 15:52
Hi Annet,
Sorry for the delay in replying, I had a really busy week at work so just haven’t had chance to check anything until this evening! I will answer each question in turn below:
– you mentioned torasemide as a rescue diuretic. And you prefer bid dosing? Why is that? I have used it but only use bid dosing if on higher dosages (>0.6mg/kg). How do you swap over from fur to torasemide in stable and unstable patient?
You can use torasemide as a first line diuretic once a day, and I do do that if the animal is tricky to medicate. I use torasemide in my stage D though normally. It has been shown in several studies that it has a t1/2 of about 10 hours so we use it twice daily to try and maintain both plasma levels and renal levels. We take the total daily dose of furosemide e.g. 10/mg/kg/day, and divide that by 1/10th-1/20th dose and then split that into two for BID dosing. We tend to use IV furosemide in an unstable patient before transitioning to torasemide, and I would only swap from furosemide to torasemide orally if the RRR were mildly elevated or we were struggling to control congestion, with the need of escalating the frusemide dose quickly.And you mentioned you can use furosemide cri? How do you do that? Which dose? And just furosemide or i vaguely remember to dilute it with hypertonic saline and dextrose?
We use it after a 2mg/kg IV bolus, then swap to CRI at 0.5-1mg/kg/hr. You tend to dilute it in D5W to keep it iso-osmolar and remember it is light sensitive!
-xrays… i dont do them much anymore since t pocus…? Is that wrong? And did you say you could have no b lines but still be in chf? I usually use microconex abd probe but can you use a phased array heart probe too?
Not wrong no, I POCUS but is an animal isn’t responding as I think they should then I will radiograph them to make sure I haven’t missed something. Micro-convex probes can be better to pick up B-lines but you can use phased-array too. B-lines should be present usually in CHF, but if you have an animal treated for CHF then there could only be 1 or 2 and that can also be normal!
– in lily’s case you mentioned most likely she’s got PH ? I assume this doesnt need treatment with sildenafil unless causing syncopes?
We don’t treat PH in stage C/D dogs usually before we try and control their congestion. You can overload the LA in theory and worsen CHF. However, if we optimise treatment and the PH remains then we might include sildenafil if they are symptomatic or if the Tr velocity is high on echo. They don’t have to be syncopal for us to use it.
– is telmisartan safe in heartdisease? Mvd st b2? And what about if in chf? I wondered if you could use that to treat the hypertension in stead of amlodipine? I assume amlodipine safer as already on benazepril?
You could use telmisartan. I am not aware of any papers that looks at their use in CHF in dogs. We don’t use ACEi in stage B2 so I don’t see why we would use telmisartan in these cases either. You could use it to treat the hypertension, but amlodipine is ‘better’ at reducing systemic hypertension usually so that would be our first line. Amlodipine also reduces afterload to a greater extent, so if a stage C dog was on an ACEi already and then developed hypertension amlodipine would be chosen and would hopefully reduce afterload enough to even reduce MR and LAP!
Hope that all makes sense.
Liz
Replying to Annet Krabbenborg 16/01/2026 - 16:24
Hi Annet,
It is common to have more than 1 congenital abnormality, but CTD is pretty rare. I have only seen a handful of cases. They usually respond well to balloon and RCHF resolves, they generally carry a good prognosis. PS will probably be the one causing the issue (if CTD was treated successfully) and if the dog is in RCHF at one years of age the prognosis is not great. We have no data on prognosis, but I’d say anecdotally that the dog will be unlikely to reach 2 yrs old. If there are no financial limitations then a second procedure could be considered, but this depends on what is causing the RCHF – is it the PS, the CTD or a combination of both?
Liz
Hi Svetlana,
I don’t really like looking for a PDA from the right parasternal view as it is very difficult to distinguish it from the LPA as you say. If we do see one it is mainly through having continuous flow on colour Doppler and then being able to demonstrate a continuous flow on spectral Doppler. That being said, it is always at an angle for me so I prefer to move to the left cranial view!
Pulmonary insufficiency should look like a jet of red originating from the pulmonic valve, not from near the branch of the PA, so should be very different. You would also hear a characteristic continuous murmur. If there is bidirectional or R-L flow then you have more of a difficult time seeing a PDa on 2D and colour – you would need to find evidence for pulmonary hypertension and then a rule out, using contrast study, would be a R-L shunt in a young animal.
If you have a PDA and PS then this can be tricky, you should still have a continuous murmur. When you interrogate the PA you should still see flow that occurs in diastole and systole – this is where moving frame by frame with an ECG is really important.
Hope that helps!
Liz
Replying to Janet Lewis 07/01/2026 - 20:43
Hi Janet,
How interesting! I think it is most likely to be a neoplasm if it is mainly associated with the wall and in a dog with that history – myxomas tend to occur in the LA/LV but not beyond possibility that it could be that. I have also seen RA chemodectomas and other weird and wonderful things. A would think a clot and endocarditis are less likely but you do right I think to provide multi-modal therapy. Also worth evaluating urine UPC? If we think it could be a clot.
Let me know how you get on with it!
Liz
Replying to Annet Krabbenborg 09/01/2026 - 14:57
Hi Annet,
Sadly not. June Boon’s book on echocardiography has tables of some of them in, otherwise you end up searching for them separately. I then print them out and have them in a folder in my room. The breeds we most commonly see are:
English springer spaniels
Whippets/ other sight hounds
Doberman
Boxer
Lab
Great DaneMost of the giant breeds have papers. Sorry that isn’t much help for you.
Liz
-
AuthorPosts